

針對在線學(xué)習(xí)版塊做簡單的介紹,文字信息長度不可超過兩行
Glaucoma is a disease that damages your eye’s optic nerve. It usually happens when fluid builds up in the front part of your eye. That extra fluid increases the pressure in your eye, damaging the optic nerve.
Glaucoma is a leading cause of blindness for people over 60 years old. But blindness from glaucoma can often be prevented with early treatment.
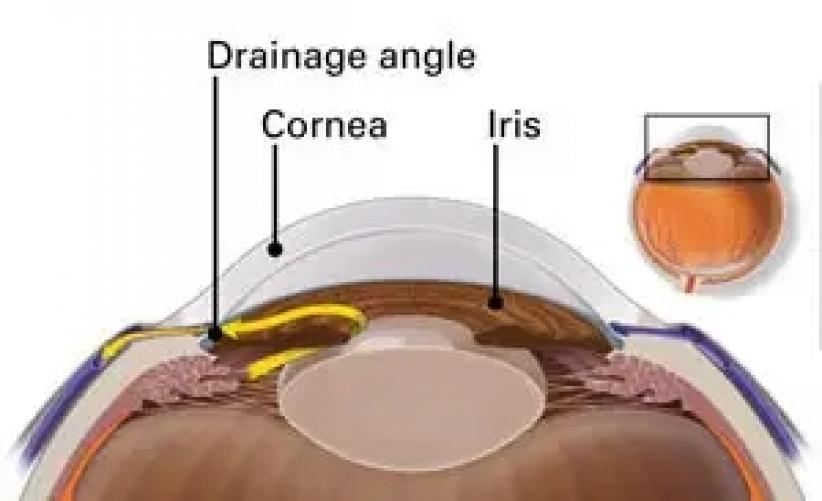
Your eye constantly makes aqueous humor. As new aqueous flows into your eye, the same amount should drain out. The fluid drains out through an area called the drainage angle. This process keeps pressure in the eye (called intraocular pressure or IOP) stable. But if the drainage angle is not working properly, fluid builds up. Pressure inside the eye rises, damaging the optic nerve.
If the drainage angle is blocked, fluid cannot flow out of the eye, causing pressure to increase.
The optic nerve is made of more than a million tiny nerve fibers. It is like an electric cable made up of many small wires. As these nerve fibers die, you will develop blind spots in your vision. You may not notice these blind spots until most of your optic nerve fibers have died. If all of the fibers die, you will become blind.
There are two major types of glaucoma.
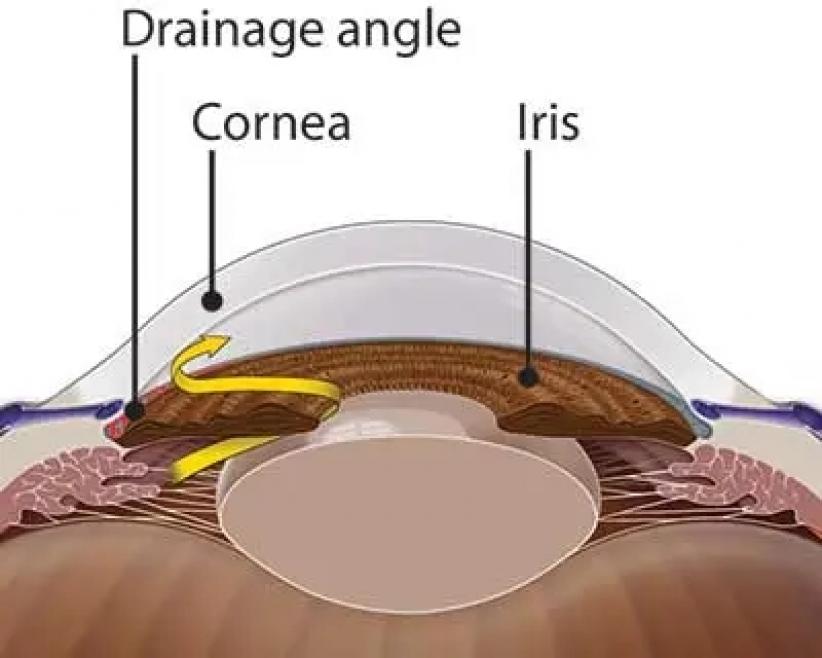
This is the most common type of glaucoma. It happens gradually, where the eye does not drain fluid as well as it should (like a clogged drain). As a result, eye pressure builds and starts to damage the optic nerve. This type of glaucoma is painless and causes no vision changes at first.
Some people can have optic nerves that are sensitive to normal eye pressure. This means their risk of getting glaucoma is higher than normal. Regular eye exams are important to find early signs of damage to their optic nerve.
This type happens when someone’s iris is very close to the drainage angle in their eye. The iris can end up blocking the drainage angle. You can think of it like a piece of paper sliding over a sink drain. When the drainage angle gets completely blocked, eye pressure rises very quickly. This is called an acute attack. It is a true eye emergency, and you should call your ophthalmologist right away or you might go blind.
Here are the signs of an acute angle-closure glaucoma attack:
Your vision is suddenly blurry
You have severe eye pain
You have a headache
You feel sick to your stomach (nausea)
You throw up (vomit)
You see rainbow-colored rings or halos around lights
Many people with angle-closure glaucoma develop it slowly. This is called chronic angle-closure glaucoma. There are no symptoms at first, so they don’t know they have it until the damage is severe or they have an attack.
Angle-closure glaucoma can cause blindness if not treated right away.
With open-angle glaucoma, there are no warning signs or obvious symptoms in the early stages. As the disease progresses, blind spots develop in your peripheral (side) vision.
Most people with open-angle glaucoma do not notice any change in their vision until the damage is quite severe. This is why glaucoma is called the “silent thief of sight.” Having regular eye exams can help your ophthalmologist find this disease before you lose vision. Your ophthalmologist can tell you how often you should be examined.
People at risk for angle-closure glaucoma usually show no symptoms before an attack. Some early symptoms of an attack may include blurred vision, halos, mild headaches or eye pain. People with these symptoms should be checked by their ophthalmologist as soon as possible. An attack of angle-closure glaucoma includes the following:
severe pain in the eye or forehead
redness of the eye
decreased vision or blurred vision
seeing rainbows or halos
headache
nausea
vomiting
People with "normal tension glaucoma" have eye pressure that is within normal ranges, but show signs of glaucoma, such as blind spots in their field of vision and optic nerve damage.
Some people have no signs of damage but have higher than normal eye pressure (called ocular hypertension). These patients are considered "glaucoma suspects" and have a higher risk of eventually developing glaucoma. Some people are considered glaucoma suspects even if their eye pressure is normal. For example, their ophthalmologist may notice something different about their optic nerve. Most glaucoma suspects have no symptoms. That is why you need to be carefully monitored by your ophthalmologist if you are a glaucoma suspect. An ophthalmologist can check for any changes over time and begin treatment if needed.
Pigment dispersion syndrome (PDS) happens when the pigment rubs off the back of your iris. This pigment can raise eye pressure and
lead to pigmentary glaucoma. Some people with PDS or pigmentary glaucoma may see halos or have blurry vision after activities like jogging or playing basketball
See your ophthalmologist if you have these or other symptoms.
Some people have a higher than normal risk of getting glaucoma. This includes people who:
have high eye pressure
are farsighted or nearsighted
have had an eye injury
use long-term steroid medications
have corneas that are thin in the center
have thinning of the optic nerve
have diabetes, migraines, high blood pressure, poor blood circulation or other health problems affecting the whole body
are over age 40
have family members with glaucoma
are of African, Hispanic, or Asian heritage
Talk with an ophthalmologist about your risk for getting glaucoma. People with more than one of these risk factors have an even higher risk of glaucoma.
The only sure way to diagnose glaucoma is with a complete eye exam. A glaucoma screening that only checks eye pressure is not enough to find glaucoma.
During a glaucoma exam, your ophthalmologist will:
measure your eye pressure
inspect your eye's drainage angle
examine your optic nerve for damage
test your peripheral (side) vision
take a picture or computer measurement of your optic nerve
measure the thickness of your cornea
Glaucoma has no symptoms in its early stages. In fact, half the people with glaucoma do not know they have it! Having regular eye exams can help your ophthalmologist find this disease before you lose vision. Your ophthalmologist can tell you how often you should be examined.
Glaucoma damage is permanent—it cannot be reversed. But medicine and surgery help to stop further damage. To treat glaucoma, your ophthalmologist may use one or more of the following treatments.